Lipoprotein(a)
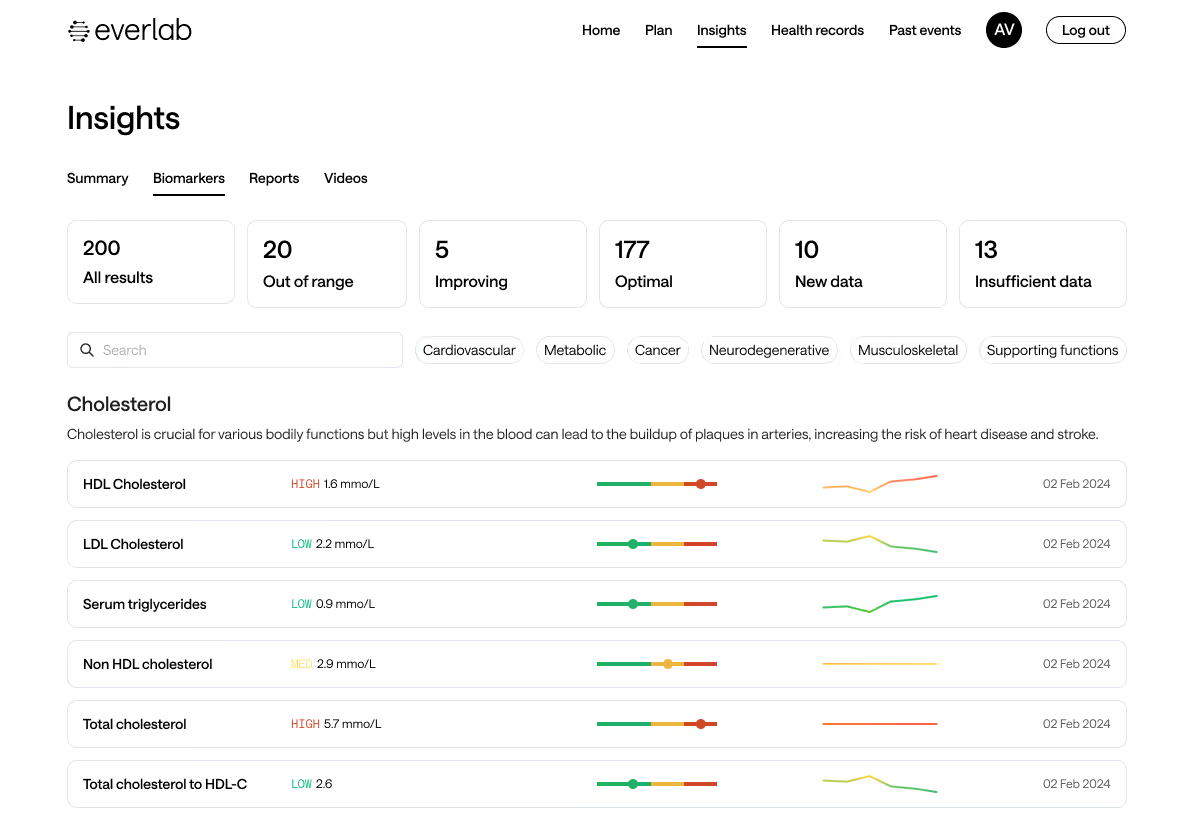
Your cholesterol levels only tell part of the story. Lipoprotein(a) is a key genetic marker that can significantly impact your cardiovascular health. At Everlab, we include Lp(a) testing in our comprehensive health assessments to help you understand your risks and take actionable steps toward a longer, healthier life.

Lp(a): A Genetic Marker For Cardiovascular Health
What:
Blood Biomarker
Tests for:
Cardiovascular Risk
Referral:
Required
Member cost:
$25
What Is Lipoprotein(a) and Why Should You Care?
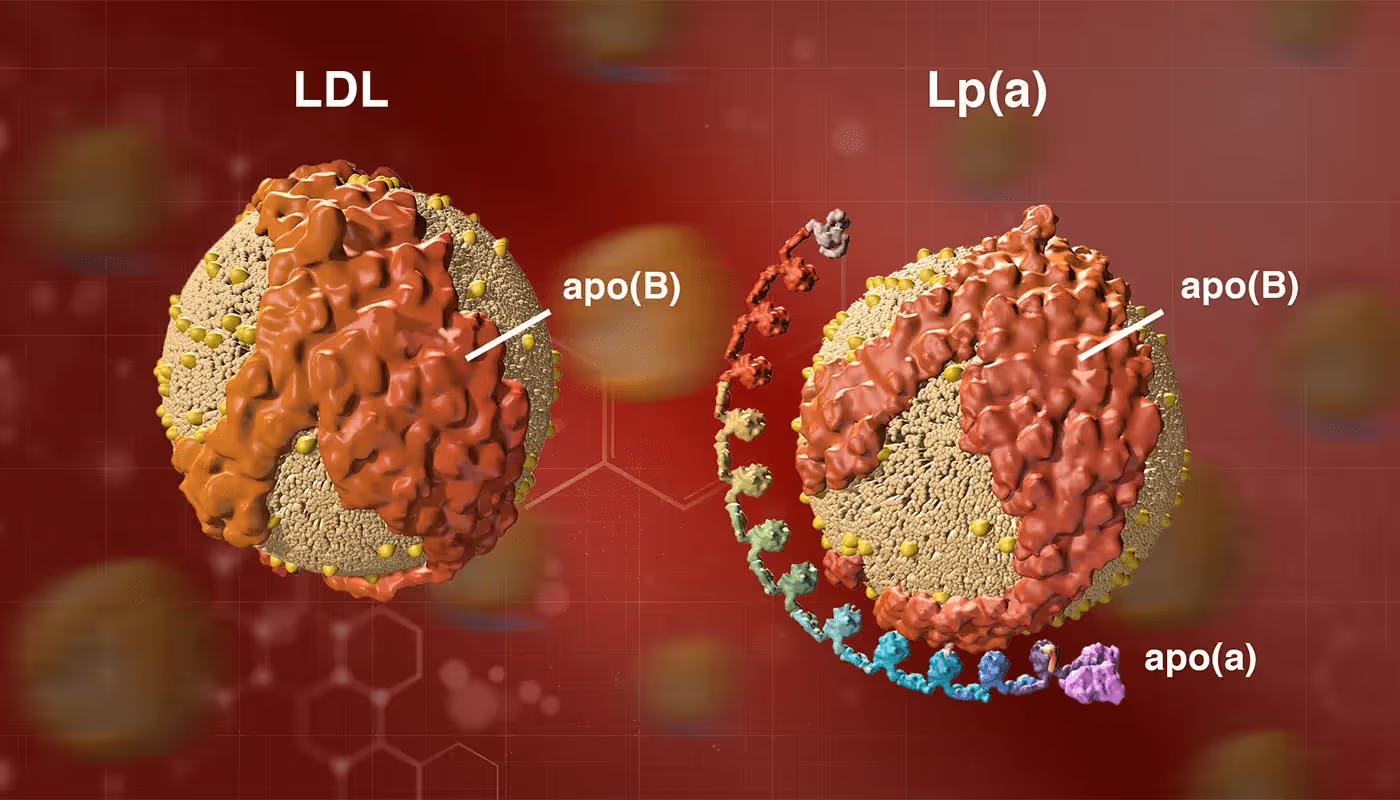
Lipoprotein(a), or Lp(a), is a type of cholesterol-carrying particle in your blood. It’s similar to LDL (“bad” cholesterol) but with an extra protein called apolipoprotein(a). Elevated lipoprotein(a) levels are an independent risk factor for heart disease, stroke, and aortic valve stenosis—even if your other cholesterol levels are normal. Testing for elevated lipoprotein(a) is crucial as it can help diagnose these conditions and identify individuals at higher risk, especially since high levels are often hereditary and not routinely tested.
Unlike LDL, which is influenced by diet and lifestyle, Lp(a) is mostly genetic. That means if you have high levels, they likely won’t decrease with the usual cholesterol-lowering strategies like diet and exercise. However, there are still ways to manage your risk.
How Is Lipoprotein(a) Measured?
An Lp(a) test is a simple blood test that measures how much Lp(a) is circulating in your body, emphasising its importance in assessing heart disease and stroke risk. It’s not included in standard cholesterol tests, so you have to request it separately.
Some labs report Lp(a) in grams per litre (g/L), while others use nanomoles per litre (nmol/L). The difference is important because nmol/L measures the number of particles, whereas g/L measures their mass. Some experts recommend using nmol/L for greater accuracy, as different Lp(a) particles vary in size and density.
Lipoprotein(a) vs. ApoB: What’s the Difference?
Both Lp(a) and apolipoprotein B (ApoB) are markers of cardiovascular risk, but they measure different things:
- Lp(a): A specific type of lipoprotein with a genetic component, strongly linked to heart disease.
- ApoB: A measurement of the total number of LDL and other atherogenic (plaque-building) particles in your blood.
If you want a complete picture of your cardiovascular risk, testing both Lp(a) and ApoB is a smart move. While high ApoB indicates a large number of LDL particles that can contribute to plaque build-up, high Lp(a) suggests an additional layer of inherited risk that might not respond to standard cholesterol-lowering approaches.
Why Test for Lp(a)?
Most people have never heard of Lp(a) because it’s not part of routine cholesterol screening. But knowing your levels can be life-changing, especially if you have:
- A family history of early heart disease (before 60 in men, 65 in women).
- A personal history of heart attack or stroke despite normal cholesterol levels.
- High LDL cholesterol that doesn’t respond well to statins.
- Unexplained heart disease despite a healthy lifestyle.
- A family history of premature heart disease, making it crucial to screen for elevated Lp(a) levels to identify high-risk individuals.
What Affects Lp(a) Levels?
Unlike LDL cholesterol, which is influenced by diet, exercise, and medications, Lp(a) is almost entirely genetic. That means:
- Lifestyle changes won’t significantly lower it.
- Your levels remain stable throughout life.
- If your parents have high Lp(a), you’re more likely to as well.
The only exception? Hormone changes—postmenopausal women often see a rise in Lp(a) levels. Certain inflammatory conditions, kidney disease, and liver dysfunction may also affect Lp(a) levels, though research is still evolving in this area. Elevated Lp(a) levels are also associated with increased risks of high blood pressure and high cholesterol, making it important to work with a physician to create a heart-healthy living plan.
How to Prepare for an Lp(a) Blood Test
An Lp(a) test requires little preparation. Unlike standard cholesterol tests, which often require fasting, you don’t need to fast before this test.
However, to ensure accurate results:
- Follow your doctor’s instructions on medications.
- Stay hydrated—drinking water can help make your veins easier to access.
- Avoid alcohol and heavy meals before your test, just to be safe.
Understanding Your Lp(a) Test Results
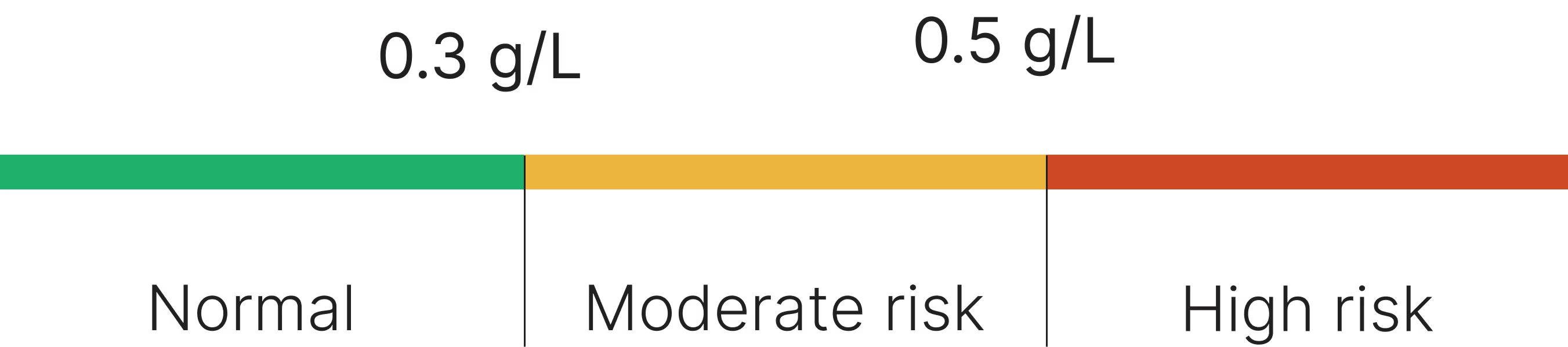
Less than 0.3 g/L: Normal
0.3 g/L - 0.5 g/L: Moderate Risk
Above 0.5 g/L: High Risk
If your levels are high, don’t panic—having high Lp(a) doesn’t mean you will definitely have a heart attack. But it does mean you have a higher risk of cardiovascular diseases and should take extra steps to manage other risk factors.
Risks and Limitations of the Lp(a) Test
While an Lp(a) test is a valuable tool, it’s not a perfect predictor of heart disease. Consider:
- It’s only one piece of the puzzle—other factors like LDL, ApoB, and lifestyle still matter.
- It won’t tell you if you already have plaque build-up—other tests, like a coronary calcium scan, can assess this.
- There’s no universal treatment—since diet and exercise don’t lower Lp(a), many doctors focus on managing overall cardiovascular risk instead.
How Lp(a) Affects Long-Term Cardiovascular Disease
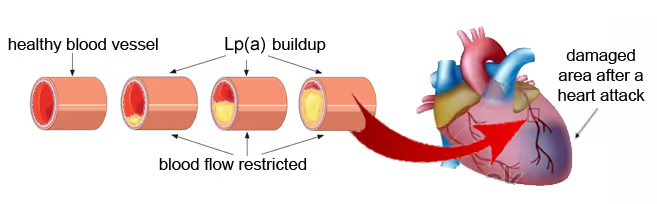
High Lp(a) levels can double or triple your risk of cardiovascular events. Over time, elevated Lp(a) can contribute to:
- Atherosclerosis (plaque build-up in arteries)
- Heart attack and stroke
- Aortic valve disease
- Blood clots (increased likelihood due to elevated Lp(a) levels)
Because it’s a lifelong risk factor, it’s crucial to monitor your levels and take proactive steps to reduce your overall cardiovascular risk.
What to Do If You Have Elevated Lipoprotein(a)
While there are currently no FDA-approved drugs specifically targeting Lp(a), some emerging treatments like siRNA-based therapies (e.g., Pelacarsen) show promise in significantly reducing Lp(a) levels. Existing cholesterol-lowering medications, such as PCSK9 inhibitors, may modestly lower Lp(a) by 20-30%, but their primary benefit is in lowering LDL cholesterol.
Since lifestyle changes don’t directly lower Lp(a), your focus should be on reducing other risk factors:
- Lower LDL cholesterol – Statins won’t lower Lp(a), but they reduce other harmful particles.
- Consider PCSK9 inhibitors – These newer cholesterol-lowering drugs can help in some cases.
- Consider niacin (under medical supervision) – Though not widely recommended, some studies suggest it may help.
- Manage blood pressure and inflammation – Lifestyle and medication can help.
- Prioritise cardiovascular fitness – Exercise may not lower Lp(a), but it strengthens your heart and arteries.
If your levels are high, your doctor may recommend more frequent cardiovascular screenings. High lipoprotein (a) levels can indicate a greater risk for heart and blood vessel disease, even if your cholesterol numbers are normal. Discussing these risks with your provider is crucial for effective management.
Take Control Of Your Lp(a) Levels
Lipoprotein(a) is a crucial but often overlooked marker for cardiovascular disease. Since Lp(a) levels are largely genetic and difficult to modify, early detection is key to managing risk. Understanding your Lp(a) levels allows healthcare providers to develop personalised prevention strategies, focusing on reducing other cardiovascular risk factors. At Everlab, we provide not just testing but actionable insights, helping you take control of your heart health and longevity.


imaging

biomarkers

sterols
Book a Free Discovery Call
Join 20,000+ Australians improving their health with proactive, personalised healthcare.