Continuous Glucose Monitor (CGM)
Continuous glucose monitoring plays a critical role in modern diabetes care by offering real-time insights into glucose fluctuations. Even with an HbA1c level of 5.6%—which falls outside the diabetic and prediabetic ranges—managing blood glucose levels and minimising glucose variability is crucial for your overall health. By achieving more stable blood glucose, you can experience improved energy levels, a reduced risk of developing diabetes, and better weight management. The Australian Government supports access to CGM products through initiatives like the National Diabetes Services Scheme (NDSS).

Continuous Glucose Monitor (CGM) In Australia, Get Tested Today
What:
Continuous Glucose Monitor
Tests for:
Daily glucose variability
Referral:
Only if claiming rebate through NDSS
Member cost:
$100 - $700 varying by provider
Overview: CGM
What is a CGM?
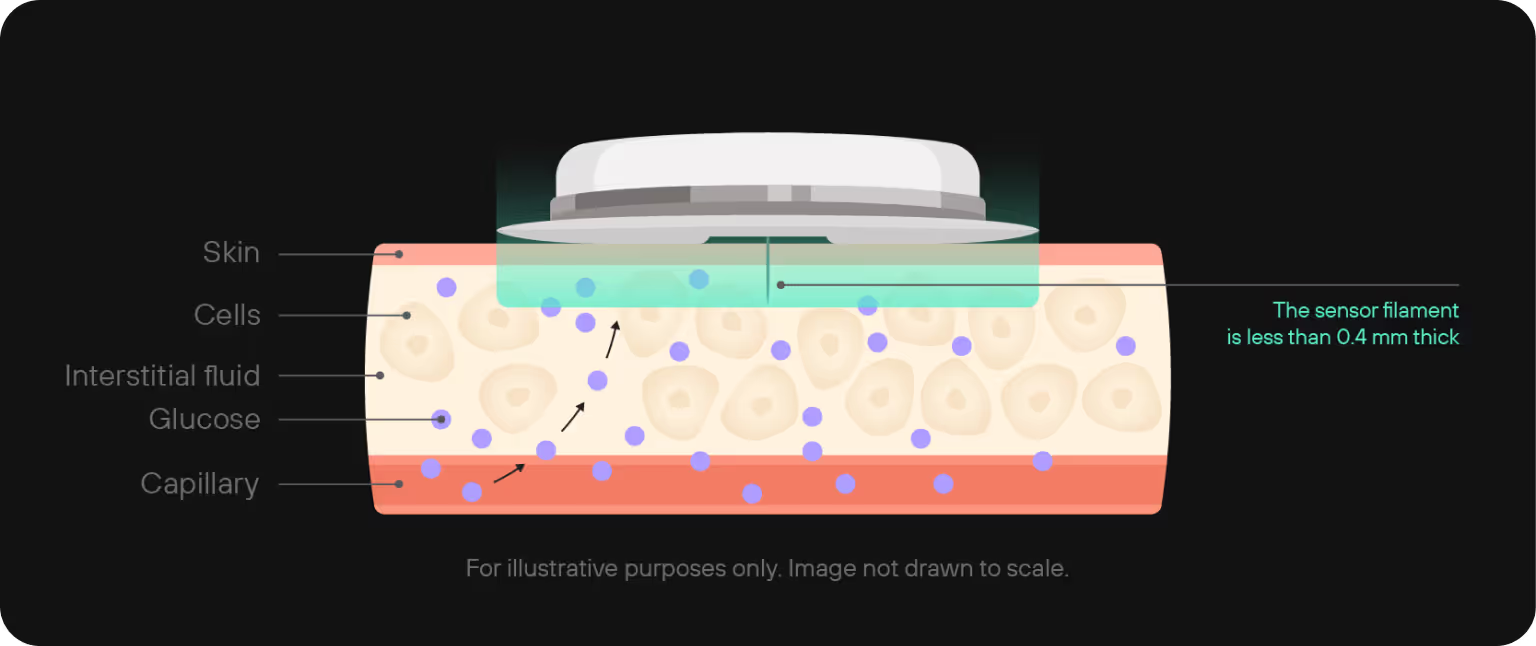
A Continuous Glucose Monitor (CGM) is a device that tracks glucose levels in real-time throughout the day and night. It uses a small sensor inserted under the skin to measure glucose in the interstitial fluid. This sensor sends your data to a reader, updating glucose readings every few minutes. The wearable device enables individuals with diabetes to monitor their glucose levels in real-time and over extended periods. CGMs provide valuable insights into glucose trends and patterns, which help users manage their diabetes more effectively. They can also alert users to high or low blood sugar levels, reducing the risk of dangerous swings. Unlike traditional blood glucose meters that require frequent fingersticks, CGMs offer continuous monitoring with fewer manual tests. CGMs are especially beneficial for individuals with type 1 diabetes or those with type 2 diabetes who need intensive monitoring.
How does a CGM work?
CGMs provide real-time glucose readings by gathering glucose data, showing current levels and trends over time. They alert users to rising or falling glucose levels, enabling timely adjustments to diet, exercise, or insulin. This continuous data helps users avoid dangerous highs (hyperglycaemia) and lows (hypoglycaemia), and is also critical for doctors to take preventative measures against diabetes. Additionally, CGMs offer a complete picture of glucose levels, enhancing glucose control and assisting individuals in making informed lifestyle choices.
The technology behind a CGM involves a small sensor that sits just under the skin—usually on the arm or abdomen. This sensor measures glucose in the interstitial fluid and sends the data wirelessly to a receiver or smartphone. Most sensors are applied with a quick, almost painless applicator and stay in place for 7 to 14 days before needing replacement.
Once set up, the system runs in the background, continuously collecting data and providing feedback throughout the day and night. Users can view trends, receive alerts, and track how their glucose responds to meals, sleep, workouts, and stress in real-time. This makes CGMs particularly valuable not just for those with diabetes, but also for people interested in improving their metabolic health and energy levels.
For those searching for a continuous glucose monitor in Australia, or comparing options for a CGM in Australia, many of today’s devices are compatible with mobile apps, making it easy to stay in control wherever you are.
Benefits of Continuous Glucose Monitors
- Improved Glycaemic Control
CGMs help you spend more time in your target glucose range (Time in Range), reducing both highs and lows. They’ve been shown to lower HbA1c by 0.5% or more without increasing the risk of hypoglycaemia. This means better long-term outcomes with fewer complications. - Fewer Hypoglycaemic Events
Real-time alerts notify you if your glucose is dropping too low or spiking too high, so you can act early. This is especially helpful during sleep, intense exercise, or times of stress—when traditional monitoring can fall short. - Faster, More Proactive Response
CGMs help you see how your glucose responds to meals, exercise, and sleep as it’s happening. That allows for smarter, quicker adjustments—like taking a short walk after a meal or adjusting your carb intake in real-time. - Deeper Insights Than a Meter Alone
While fingerstick meters provide one-off snapshots, CGMs show patterns, trends, and variability over 24 hours. This holistic view allows you and your healthcare team to fine-tune your treatment and lifestyle decisions with precision. - Better Long-Term Management
By analysing trends over days and weeks, CGMs help optimise insulin dosing, food timing, and activity. Over time, this can reduce the risk of serious complications like cardiovascular disease, nerve damage, and kidney failure.
Blood Glucose Meter vs. CGM
When comparing blood glucose meters to Continuous Glucose Monitors (CGMs), it’s essential to consider the distinct advantages and limitations of each device. Blood glucose meters provide accurate, instantaneous glucose readings, but they require frequent fingerstick tests, which can be painful and inconvenient. In contrast, CGMs offer continuous glucose monitoring, providing a more comprehensive understanding of glucose trends and patterns. However, CGMs may require calibration with blood glucose meters and can be more expensive. Ultimately, the choice between a blood glucose meter and a CGM depends on individual preferences, lifestyle, and diabetes management needs. Many individuals with diabetes use a combination of both devices to achieve optimal glucose control.
CGM Impact on Longevity
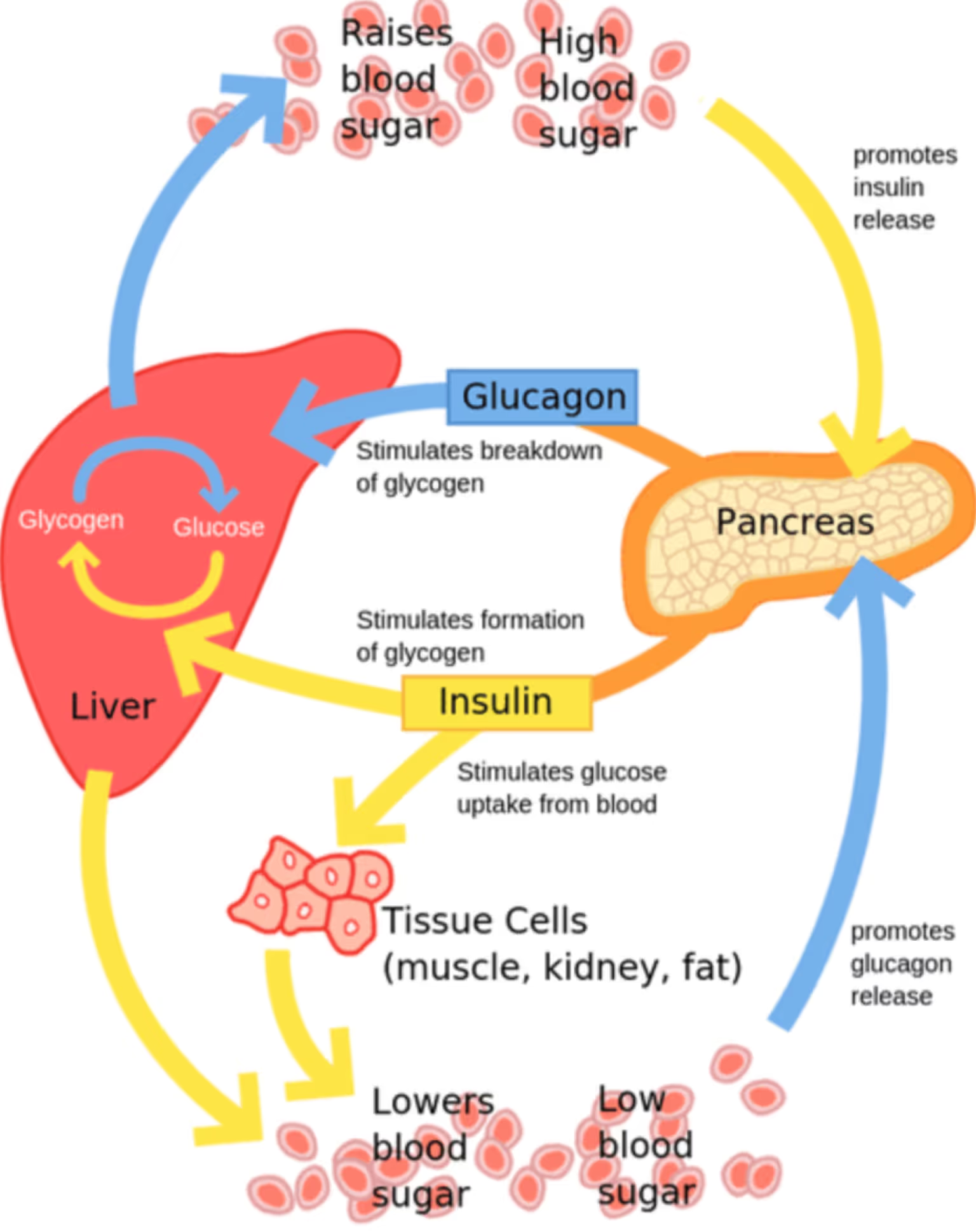
Why is measuring the amount of glucose important?
Measuring glucose levels through blood glucose monitoring is vital for detecting, managing, and preventing diabetes. Its importance extends beyond diabetes into overall metabolic health, research, and performance. Here's why it matters:
- Diabetes Management
- For individuals with diabetes, regularly monitoring blood glucose helps adjust diet, physical activity, and medication.
- Self-monitoring is a crucial part of daily management and helps maintain glucose within a healthy range.
- It helps prevent serious complications, including:
- Hypoglycaemia (low blood sugar)
- Cardiovascular disease
- Nerve damage
- Kidney failure
- Metabolic Health & Prevention
- Glucose measurement is essential for assessing insulin sensitivity.
- Consistently high or fluctuating glucose levels can signal early stages of metabolic syndrome or other health issues.
- Intermittent fasting is a promising intervention to improve insulin sensitivity and glucose control, offering a proactive tool for better metabolic health.
- Research, Clinical Trials & Performance
- Glucose monitoring is used to understand how the body responds to interventions such as:
- Dietary changes (like intermittent fasting)
- Physical exertion
- This data helps refine:
- Treatment plans
- Preventive health strategies
- Athletic performance optimisation
- Glucose monitoring is used to understand how the body responds to interventions such as:
Getting Started With Your CGM
What is the process of getting a CGM?
1. Consultation with Healthcare Provider: The first step is to discuss your interest in a CGM with your doctor, endocrinologist, or diabetes specialist. They will assess your need for a CGM based on your medical history, diabetes management goals, and current treatment plan. If a CGM is deemed appropriate, the doctor will provide a prescription for it.
2. Selecting a CGM Device: There are several CGM devices available, such as the Freestyle Libre. Your healthcare provider will help you choose the best device based on your individual needs and preferences.
3. Installation and Setup: Setting up a CGM typically involves inserting a small sensor under the skin, usually on the abdomen or the back of the arm. The sensor continuously monitors glucose levels and transmits the data to a receiver, smartphone app, or insulin pump. The installation process may be done at home or under the guidance of a healthcare professional, depending on the device and your preference.
4. Training and Monitoring: After installation, you’ll receive training on how to use the CGM, interpret the data, and troubleshoot any issues. Ongoing monitoring and regular follow-ups with your healthcare provider are important to ensure that the CGM is effectively helping manage your diabetes. Adjustments to your treatment plan may be made based on the CGM data.
5. Ongoing Use and Replacement: CGM sensors typically need to be replaced every 7 to 14 days, depending on the device. You’ll continue using the CGM as part of your diabetes management plan, with regular check-ins with your healthcare provider to review your progress and make any necessary adjustments.
What else do I need to know?
How can I interpret my CGM?
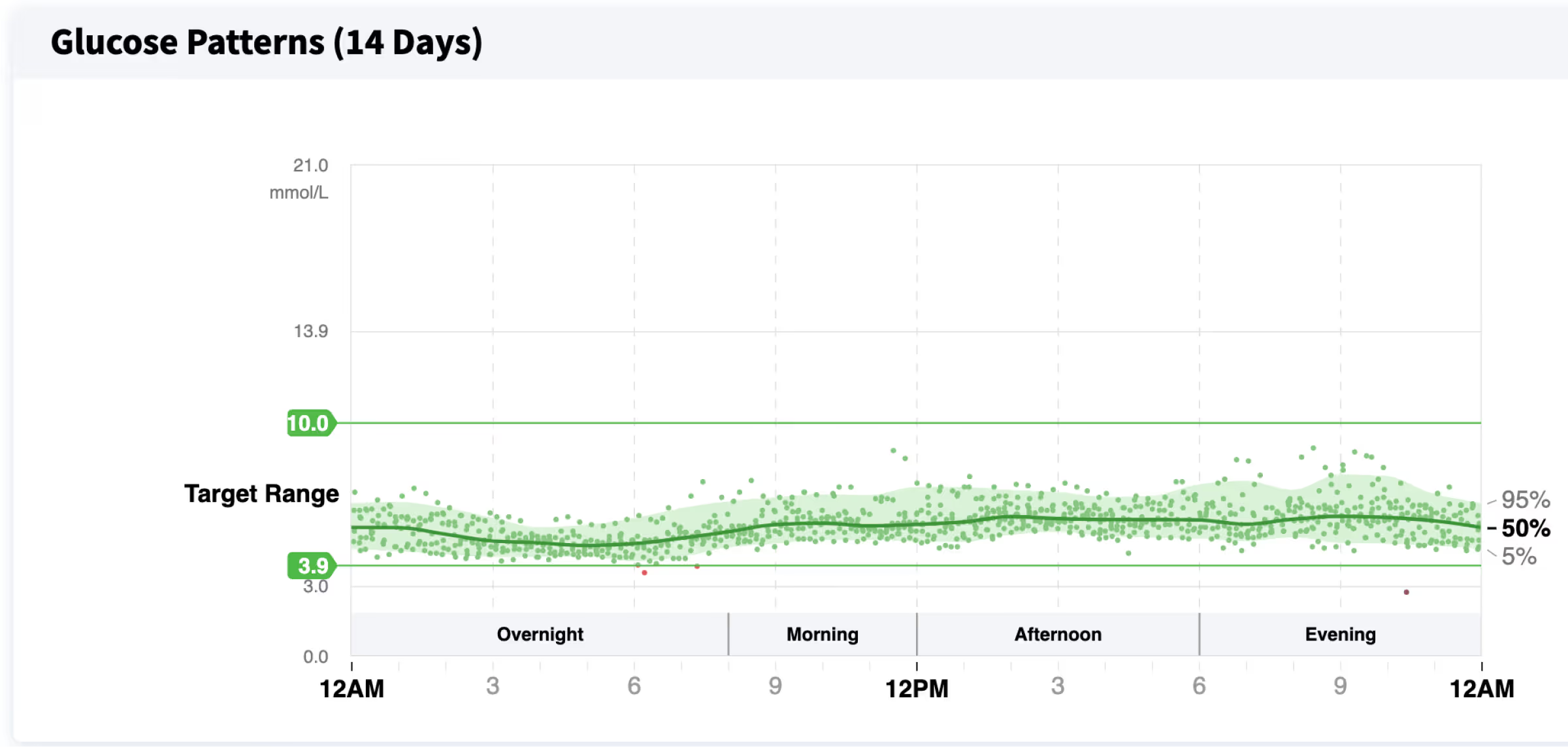
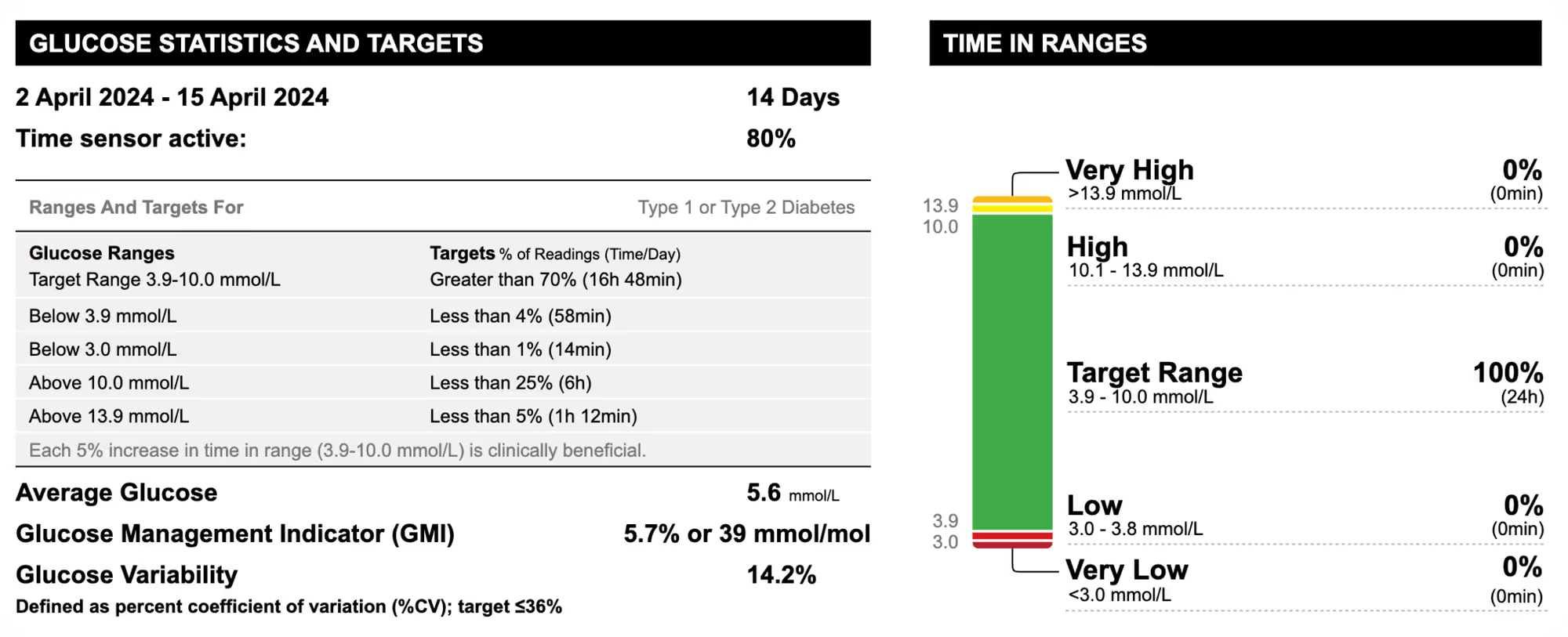
There are several key parts of the data that should be looked at, including blood glucose readings. Try having a read of the graph below!
Axes:
The horizontal axis represents the time of day, spanning from 12 AM (midnight) to 12 AM (the following midnight). The vertical axis represents average glucose levels in mmol/L ranging from 21 mmol/L to 0 mmol/L.
Target Range (3.9-10 mmol/L):
The green band represents the target glucose range, which is typically 3.9 to 10 mmol/L for most healthy individuals.
Time in Range (TIR):
The green lines within the target range (3.9-10 mmol/L) represents the percentage of time the glucose levels stayed within this desired range. Higher time in this range is generally an indicator of good glucose management.
Glucose Variability:
The broader the bands, the more variable the glucose levels. Narrower bands indicate more consistent glucose control. Glucose variability is usually measured as a %, where the lower the % the better.
Interpretation:
Look for times when the glucose levels are consistently above or below the target range. Identify patterns, such as periods of frequent highs or lows at specific times of the day. This information can help in making adjustments to diet, medication, or other lifestyle factors to achieve better glucose control. Additionally, continuous glucose monitors allow users to share data with caregivers, facilitating better health management.
Factors Affecting CGM Accuracy
The accuracy of Continuous Glucose Monitors (CGMs) can be influenced by several factors, including the type of device, sensor placement, and user technique. Interstitial fluid, which surrounds the sensor, can also impact CGM readings, as it may not always reflect blood glucose levels accurately. Additionally, certain medications, such as steroids, and lifestyle factors, like intense physical activity or dietary changes, can affect CGM accuracy. To ensure optimal performance, it’s crucial to follow the manufacturer’s instructions, calibrate the device regularly, and consult with a healthcare provider if concerns arise. By understanding the factors that can impact CGM accuracy, individuals with diabetes can take steps to minimise errors and optimise their glucose management.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
Continuous Glucose Monitoring.
https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/continuous-glucose-monitoring - Testing.com
Continuous Glucose Monitoring (CGM)
https://www.testing.com/tests/continuous-glucose-monitoring/ - Diabetes Australia – National Diabetes Services Scheme (NDSS)
Access to Continuous Glucose Monitoring
https://www.ndss.com.au/living-with-diabetes/managing-diabetes/continuous-glucose-monitoring/ - Mayo Clinic
Blood sugar testing: Why, when and how.
https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/blood-sugar/art-20046628
Why is a CGM so important?
Ultimately, with the right CGM and blood data, healthcare providers can triangulate an accurate diagnosis and prescribe specific interventions tailored to stabilising your blood glucose levels. CGM can also improve diabetes-specific patient-reported outcomes, including diabetes distress, by enabling better self-management and engagement with glycaemic data. Some simple tweaks include eating whole fruits instead of processed or juiced versions, lowering the GI of your carbs by adding acidity, and walking for 30 minutes after meals. Recognising symptoms of high or low blood sugar levels is crucial; if you experience any concerning symptoms, contact your healthcare provider.
Additional FAQs


imaging

biomarkers

sterols
Book a Free Discovery Call
Join 20,000+ Australians improving their health with proactive, personalised healthcare.