The Ultimate Guide to Fasting Insulin: Why It Matters for Your Health
Your blood sugar levels only tell part of the story. Fasting insulin is a key biomarker that provides a clearer picture of your metabolic health and insulin sensitivity. At Everlab, we include fasting insulin testing in our comprehensive health assessments to help you detect early signs of insulin resistance and take proactive steps toward a healthier, longer life.

Fasting Insulin: A Better Marker for Metabolic Health
What:
Blood biomarker
Tests for:
Metabolic and cardiovascular risk
Referral:
Required
Member cost:
Part of larger blood panel
What is Fasting Insulin?
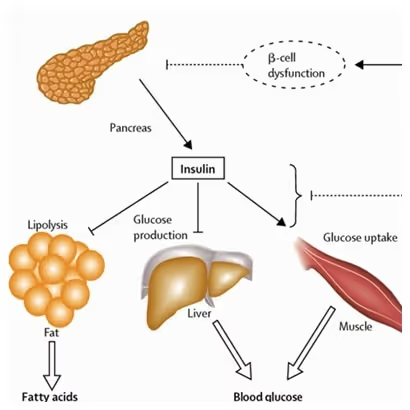
Fasting insulin is a measure of the amount of insulin in your blood after an extended period without eating, typically 8-12 hours. Insulin is a hormone produced by the pancreas that helps regulate both blood sugar and blood glucose levels by allowing cells to absorb glucose. Unlike a standard insulin blood test, a fasting insulin test provides a clearer picture of how your body manages blood sugar in a fasted state, offering insight into metabolic health.
How is Fasting Insulin Measured?
A fasting insulin test is a simple blood test that requires overnight fasting. A healthcare provider will take a blood sample, usually from a vein in your arm, and send it to a laboratory for analysis. The test results indicate how much insulin your pancreas produces when no food is present in your system, helping assess insulin sensitivity and metabolic function. Fasting insulin tests are part of a broader category of insulin tests used to monitor metabolic health, including detecting insulin resistance and chronic diseases like prediabetes and type 2 diabetes.
Why is insulin tested fasted?
Fasting insulin is tested in a fasted state because it provides a clear, unaltered measure of your baseline insulin production without the influence of recent meals. After eating, insulin levels naturally rise in response to glucose intake, making it difficult to assess how efficiently your body regulates blood sugar at rest. Testing in a fasted state ensures that the results accurately reflect your body’s insulin sensitivity and metabolic function.
What is Insulin Sensitivity?
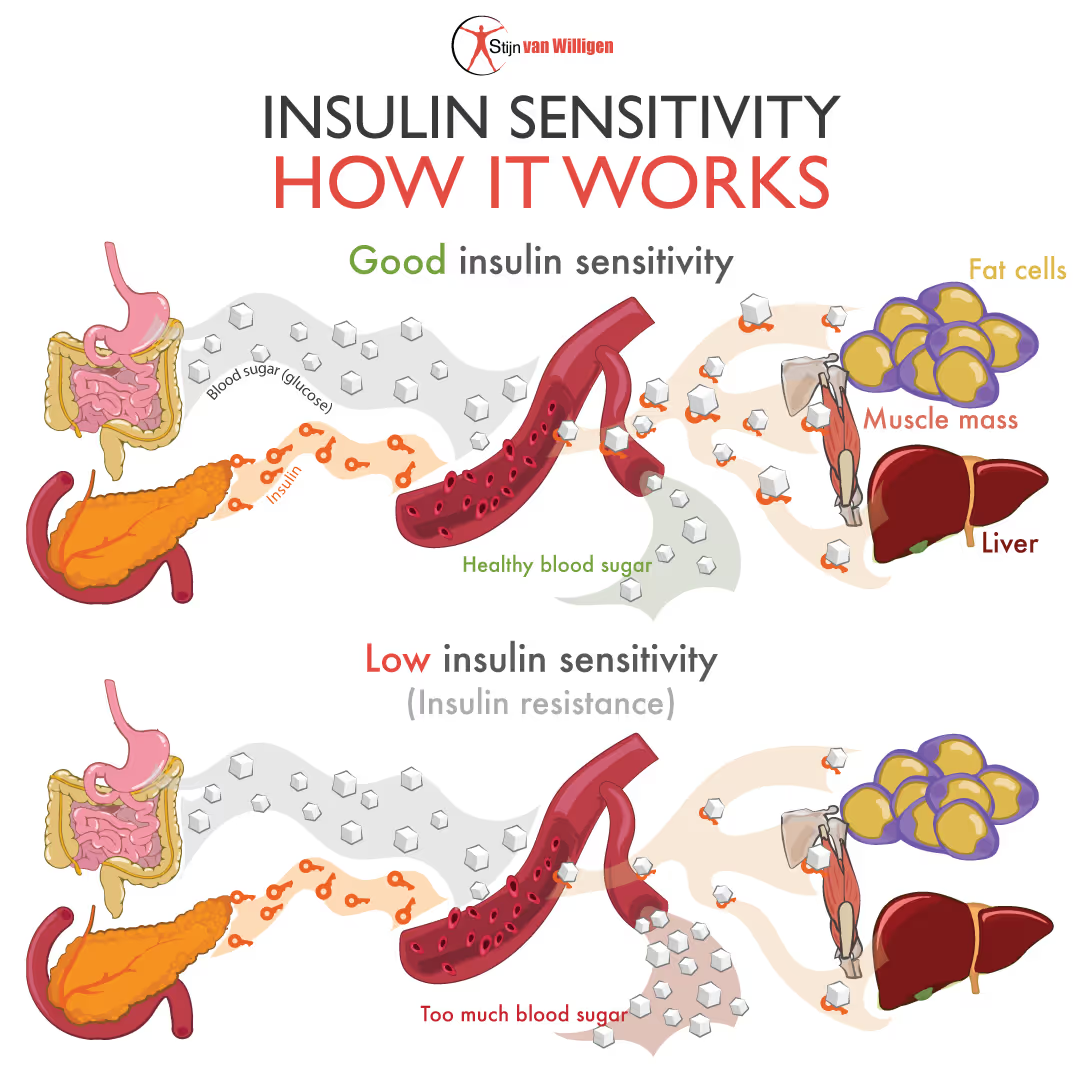
Insulin sensitivity refers to how effectively your body’s cells respond to insulin, the hormone responsible for regulating blood sugar levels. When insulin sensitivity is high, your cells efficiently absorb glucose from the bloodstream, keeping blood sugar levels stable and reducing the demand for excess insulin production. On the other hand, low insulin sensitivity—known as insulin resistance—means your cells are less responsive to insulin, leading to higher insulin and blood sugar levels over time.
The Relationship Between Insulin Sensitivity and Fasting Insulin
Fasting insulin is a direct indicator of insulin sensitivity. When insulin sensitivity is high, your body needs only a small amount of insulin to regulate blood sugar levels, resulting in low fasting insulin levels. Conversely, when insulin sensitivity is low (insulin resistance), the pancreas has to produce more insulin to compensate for the reduced effectiveness of insulin in the cells. This leads to elevated fasting insulin levels, which can signal early metabolic dysfunction even before blood sugar levels become abnormal.
Why is Fasting Insulin Important for Your Health?
High fasting insulin levels can lead to elevated blood glucose levels and increased risk of type 2 diabetes, obesity, and cardiovascular disease, as the body’s cells become less responsive to insulin.
Low fasting insulin levels, on the other hand, could indicate pancreatic dysfunction or other metabolic disorders. Maintaining optimal fasting insulin levels is essential for overall health, longevity, and disease prevention.
Why Should You Test Your Fasting Insulin Levels?
Fasting insulin is one of the earliest markers of insulin resistance—often before blood sugar levels become abnormal. Testing can help identify potential metabolic issues before they progress to conditions like type 2 diabetes.
High fasting insulin levels are associated with increased risks of chronic diseases due to imbalances in insulin and glucose levels, including obesity, cardiovascular disease, Alzheimer’s disease, and polycystic ovary syndrome (PCOS). Regular testing allows for early intervention and lifestyle modifications.
By tracking fasting insulin levels, you can take proactive steps to improve metabolic health, reduce disease risk, and enhance overall well-being through diet, exercise, and other lifestyle changes.
Factors That Affect Fasting Insulin Levels
Diet and Nutrition
- High carbohydrate and processed food intake can cause blood glucose to rise, leading to elevated insulin levels.
- A diet rich in whole foods, fibre, and healthy fats helps regulate insulin.
- Protein intake also influences insulin levels but varies based on individual needs.
Physical Activity
- Regular exercise, particularly strength training and high-intensity interval training (HIIT), improves insulin sensitivity and lowers fasting insulin levels.
Sleep and Stress
- Poor sleep and chronic stress increase insulin resistance and elevate fasting insulin levels.
- Prioritizing quality sleep and stress management techniques, such as meditation, can improve insulin regulation.
Medical Conditions
- Conditions like PCOS, metabolic syndrome, and type 2 diabetes can affect fasting insulin levels.
- Certain medications, such as steroids and antipsychotics, may also impact insulin metabolism.
- Digestive and kidney diseases, as researched by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), can also impact fasting insulin levels.
How to Prepare for a Fasting Insulin Blood Test
- Fast for 8-12 hours before the test (only water is allowed).
- Avoid high-carb meals the night before to prevent temporary insulin spikes.
- Stay hydrated with water to ensure an accurate blood draw.
- Limit intense exercise before the test, as it can temporarily alter insulin levels.
- Inform your doctor about any medications or supplements you take, as some can affect results.
Understanding Fasting Insulin Test Results
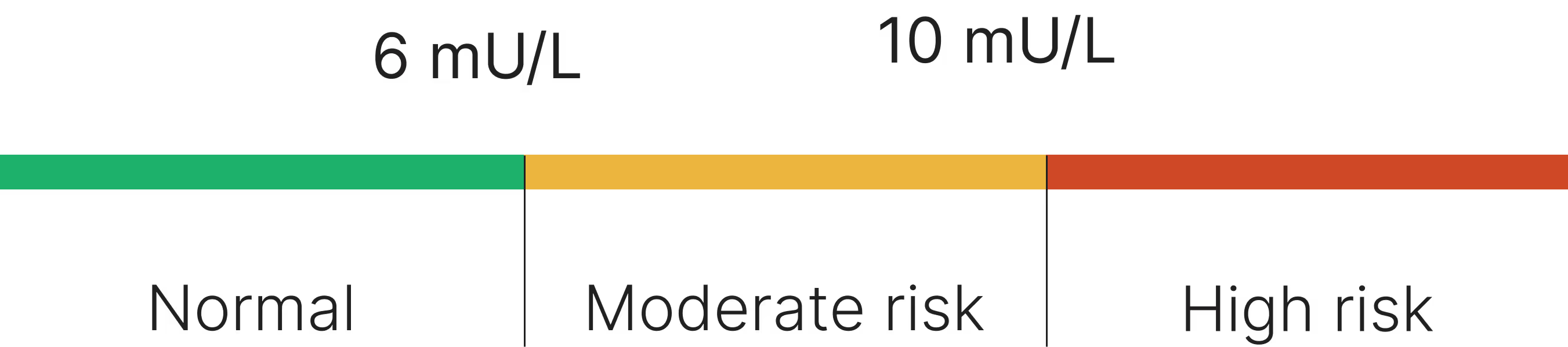
- Normal: 4-6 mU/L (micro-international units per litre)
- Moderate Risk: 6-10 mU/L
- High Risk Of Insulin Resistance: >10 mU/L
- Low: <4 mIU/L
What Do Abnormal Levels Mean?
- High fasting insulin suggests insulin resistance, which increases the risk of metabolic diseases.
- Low fasting insulin may indicate pancreatic beta-cell dysfunction or an underlying health issue, often associated with low blood glucose levels, requiring further investigation.
Risks and Limitations of the Fasting Insulin Test
- Not diagnostic on its own – Fasting insulin should be assessed alongside other tests, such as fasting glucose and HOMA-IR (Homeostatic Model Assessment of Insulin Resistance).
- Affected by lifestyle factors – Recent diet, stress, and sleep patterns can influence results.
- Variability between labs – Different labs may use slightly different reference ranges.
Long-Term Health Implications of Fasting Insulin Levels
- Persistent high fasting insulin is associated with obesity, fatty liver disease, and increased cardiovascular risk.
- Lower fasting insulin levels with good glucose control are linked to longevity and better metabolic health.
- Chronic insulin resistance can progress to prediabetes and type 2 diabetes if left unchecked.
- Too much insulin in the body can lead to conditions like hyperinsulinemia and hypoglycaemia, requiring medical attention.
How to Improve Fasting Insulin Results
Dietary Changes
- Reduce processed carbohydrates and sugar.
- Increase intake of healthy fats (avocados, nuts, olive oil) to stabilize blood sugar and glucose levels.
- Follow intermittent fasting to allow insulin levels to reset.
Exercise
- Strength training and HIIT are particularly effective at improving insulin sensitivity.
- Consistent physical activity throughout the day helps maintain balanced insulin levels.
Lifestyle Modifications
- Improve sleep quality by maintaining a consistent sleep schedule.
- Manage stress through mindfulness, meditation, or therapy.
- Maintain a healthy weight to prevent insulin resistance.
Take Control of Your Fasting Insulin Levels
Fasting insulin is one of the most powerful indicators of metabolic health and early insulin resistance. It plays a crucial role in blood sugar regulation and long-term disease risk, including diabetes, obesity, and cardiovascular disease. By understanding your fasting insulin levels, healthcare providers can detect issues before they escalate and guide you toward effective interventions. At Everlab, we help you stay ahead of disease risk with cutting-edge diagnostics and tailored health interventions.
.avif)


imaging

biomarkers

sterols
Book a Free Discovery Call
Join 20,000+ Australians improving their health with proactive, personalised healthcare.